When a multiple sclerosis relapse hits, every hour counts. Numbness spreads. Vision blurs. Walking becomes a struggle. Doctors often reach for dexamethasone - a powerful steroid - to stop the attack before it locks in. But is it truly the best choice? Or are we using an old tool because it’s familiar, not because it’s right?
What Dexamethasone Actually Does in MS
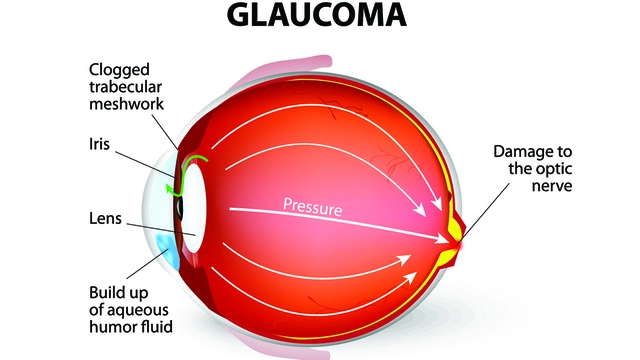
Dexamethasone is a synthetic corticosteroid, part of the same family as prednisone and methylprednisolone. It works by slamming the brakes on inflammation. In MS, the immune system attacks the protective coating around nerve fibers - myelin. That’s what causes relapses. Dexamethasone doesn’t fix the damage. It doesn’t stop MS from coming back. But it does quiet the immune system’s overreaction fast.
Unlike some other steroids, dexamethasone has a long half-life. That means one dose lasts longer. For patients, this often translates to fewer pills. A typical MS relapse protocol might involve 20 to 40 milligrams per day for 5 to 7 days, sometimes starting with a high IV dose and switching to oral. It’s not a cure. It’s a fire extinguisher.
How It Compares to Other Steroids
For decades, intravenous methylprednisolone has been the gold standard for treating MS relapses. But dexamethasone is gaining ground - not because it’s better, but because it’s easier to use.
| Steroid | Typical Dose | Route | Half-Life | Common Side Effects |
|---|---|---|---|---|
| Methylprednisolone | 500-1000 mg daily | IV | 18-36 hours | Insomnia, mood swings, stomach upset |
| Prednisone | 60-80 mg daily | Oral | 18-36 hours | Weight gain, fluid retention, high blood sugar |
| Dexamethasone | 20-40 mg daily | Oral or IV | 36-72 hours | Insomnia, elevated blood pressure, increased infection risk |
Studies show dexamethasone works just as well as methylprednisolone in reducing relapse symptoms within a week. But here’s the catch: it doesn’t change long-term outcomes. Patients still end up with the same level of disability six months later, regardless of which steroid they took. That’s because steroids don’t touch the underlying disease process. They only mask the flare-up.
Why Some Doctors Prefer Dexamethasone
For many neurologists, the appeal of dexamethasone is practical. A patient can take it at home. No hospital visits. No IV lines. No nurses to schedule. In rural areas or for people with limited mobility, that’s a game-changer.
One 2023 study from the University of California compared 217 MS patients treated with either oral dexamethasone or IV methylprednisolone. Both groups improved similarly in EDSS scores - a standard measure of disability - after 14 days. But the dexamethasone group had 68% fewer clinic visits. That’s not just convenient. It’s cost-effective.
Another advantage: dexamethasone’s longer action means less frequent dosing. A patient on prednisone might need to take pills twice a day. With dexamethasone, once-daily is often enough. Fewer pills mean fewer missed doses and better adherence.
The Hidden Costs: Side Effects You Can’t Ignore
Powerful drugs come with powerful side effects. Dexamethasone isn’t gentle. Even short courses can cause:
- Severe insomnia - some patients report sleeping only 2-3 hours a night
- Sharp spikes in blood sugar - dangerous for people with prediabetes or diabetes
- Emotional swings - anxiety, irritability, even panic attacks
- Increased risk of infections - especially fungal or bacterial
- Fluid retention - leading to swollen ankles or sudden weight gain
These aren’t rare. In a 2024 survey of 400 MS patients treated with steroids, 62% reported significant sleep disruption. Nearly half said their mood changed noticeably. One woman in the study described it as “being wired and weepy at the same time.”
And here’s something rarely discussed: dexamethasone can mask symptoms of other problems. A patient on steroids might feel better from their MS relapse - but still have a hidden urinary tract infection or pneumonia. The fever and fatigue get blamed on the MS, when they’re actually signs of something else.
Who Should Avoid It
Dexamethasone isn’t for everyone. It’s risky if you have:
- Uncontrolled diabetes
- Active infections (like tuberculosis or hepatitis B)
- History of stomach ulcers or GI bleeding
- Severe mental health conditions like bipolar disorder
- Pregnancy - it crosses the placenta and may affect fetal development
For older adults, especially those with osteoporosis, even a short course can speed up bone loss. One 2022 study found that MS patients over 60 who took steroids had a 30% higher fracture risk in the following year.
And if you’ve already taken multiple steroid courses in the past year, your body’s natural cortisol production may be suppressed. Suddenly stopping dexamethasone can trigger adrenal crisis - a life-threatening drop in blood pressure and energy.
What Comes After the Steroid Course
Taking dexamethasone for a relapse is like putting out a fire. But if the house is still burning underneath, the fire will come back.
That’s why steroids are never a standalone solution. They’re a bridge - not a destination. After the flare fades, patients need to be on a disease-modifying therapy (DMT). Drugs like ocrelizumab, natalizumab, or siponimod actually slow MS progression. They reduce the number of relapses over time. Steroids don’t do that.
Yet too many patients stop their DMTs after a steroid course because they feel “fine.” That’s a mistake. Feeling better doesn’t mean the disease is quiet. Brain scans often show new lesions forming even when symptoms disappear.
Is Dexamethasone the Future of MS Treatment?
No. But it might be part of the present.
The real future of MS treatment lies in neuroprotection and repair - drugs that stop nerve damage before it happens or help the body heal damaged myelin. Companies are testing remyelinating agents and BTK inhibitors. These could one day replace steroids entirely.
For now, dexamethasone has a role: fast, affordable, and effective for acute flares - especially when IV access is hard to get. But it’s not a magic bullet. It’s a tool. And like any tool, it’s only as good as the person using it.
If you’re considering dexamethasone for an MS relapse, ask your doctor: Why this over methylprednisolone? What are the risks for me? What comes next? Don’t accept a quick fix. Demand a plan.
Can dexamethasone cure multiple sclerosis?
No. Dexamethasone only treats the symptoms of an MS relapse by reducing inflammation. It does not stop the underlying autoimmune process that causes MS. Disease-modifying therapies (DMTs) are the only treatments proven to slow progression over time.
How long does it take for dexamethasone to work in MS?
Most patients notice improvement in symptoms like vision problems or weakness within 3 to 5 days of starting treatment. Full recovery can take up to 2 weeks. But even if symptoms disappear, the disease is still active - follow-up with your neurologist is essential.
Is oral dexamethasone as effective as IV steroids for MS relapses?
Yes, for most patients. Recent studies show oral dexamethasone works just as well as IV methylprednisolone in reducing relapse symptoms within 14 days. The main difference is convenience: oral treatment avoids hospital visits and IV lines.
What are the biggest risks of taking dexamethasone for MS?
The biggest risks include severe insomnia, spikes in blood sugar (especially dangerous for diabetics), mood changes like anxiety or depression, increased infection risk, fluid retention, and bone loss with repeated use. Sudden withdrawal after long-term use can cause adrenal crisis.
Should I take dexamethasone if I have a cold or infection?
No. Dexamethasone suppresses your immune system, which can turn a minor infection into a serious one. If you have a fever, cough, or signs of infection, tell your doctor before starting steroids. You may need to delay treatment until the infection clears.
Can I drink alcohol while taking dexamethasone for MS?
It’s best to avoid alcohol. Both alcohol and dexamethasone can irritate the stomach lining, increasing the risk of ulcers. Alcohol also worsens dexamethasone’s effects on blood sugar and sleep, making side effects more severe.
Will dexamethasone help with progressive MS, not just relapses?
No. Dexamethasone is only used for acute relapses - sudden flare-ups of symptoms. In progressive forms of MS, where damage builds slowly without clear flares, steroids have not been shown to help. Treatment focuses on symptom management and disease-modifying therapies designed for progression.
What to Do Next
If you’re facing an MS relapse and your doctor suggests dexamethasone, don’t just say yes. Ask: What’s the plan after the steroids? Are we adding or adjusting my DMT? What signs should I watch for that mean this isn’t working? What happens if I can’t tolerate the side effects?
MS treatment isn’t about one drug. It’s about a strategy. Dexamethasone has its place - but only as one piece. The real goal is staying well long-term. That means staying on your DMT, tracking your symptoms, and working with a neurologist who treats you as a person, not a case number.






Comments
Dale Yu
October 28, 2025Dexamethasone is just another corporate drug push disguised as medicine
Doctors don't care about you they care about billing codes and hospital quotas
You think this helps? It just buys time until the next breakdown
They don't want you cured they want you dependent
Kshitij Nim
October 29, 2025Actually in India we use dexamethasone more often than IV methylprednisolone because it's cheaper and accessible
Many patients can't afford hospital stays or IV infusions
And yes the side effects are real but sometimes you pick the lesser evil
Just make sure you're monitored and follow up with your neurologist
Scott Horvath
October 31, 2025so like... i took dexa last year for my relapse
felt like a zombie wired on espresso and rage
but hey at least i didn't have to go to the hospital
my cat even noticed i was different
she stayed away for three days
weird but true
anyone else feel like their emotions got hijacked?
Armando Rodriguez
November 1, 2025This is an exceptionally well-researched and balanced overview of dexamethasone use in MS relapses. The distinction between symptom management and disease modification is critical and often misunderstood by patients. The data on reduced clinic visits with oral dexamethasone is particularly compelling for resource-limited settings. I would encourage all clinicians to consider individual patient factors-including mobility, comorbidities, and access to care-when selecting steroid regimens. Thank you for emphasizing the necessity of ongoing DMT therapy post-steroid course.
jennifer sizemore
November 2, 2025Just wanted to say thank you for writing this
I was scared to start dexamethasone because of all the horror stories online
But reading this made me realize it's not about being afraid of the drug
It's about being informed and asking the right questions
My neurologist and I made a plan together and I feel way more in control now
matt tricarico
November 2, 2025Let's be honest - dexamethasone is a Band-Aid on a hemorrhage. The entire MS treatment paradigm is built on placebo-effect-driven protocols and pharmaceutical marketing. The real cure? It's been suppressed for decades. You think this is science? It's a money machine. Look at the patent filings. Look at the ghost-authorship papers. The FDA is complicit. You're being played.
Patrick Ezebube
November 3, 2025They gave me dexamethasone and then my blood sugar went through the roof
And my doc didn't even test me for prediabetes first
That's not medicine - that's chemical warfare
And now I'm told I have to take metformin for life
They knew this would happen
They just don't care
Kimberly Ford
November 4, 2025Hey Patrick - I hear you, and I'm so sorry you went through that
It's terrifying when a treatment makes you feel worse than the disease
But please don't assume your doctor didn't care - sometimes they're working with limited tools and guidelines
What helped me was keeping a symptom journal and bringing it to every appointment
It turned my care from reactive to proactive
You deserve better - and you can advocate for it
Write a comment