When you hear the word generic, you probably think of cheap pills that work just like the brand-name ones. But when it comes to biologics, that’s not the whole story. Biologics aren’t made in a lab like regular pills-they’re grown in living cells. That makes them incredibly complex. And because of that, you can’t have an exact copy. What you get instead is a biosimilar. It’s not a generic. It’s something else entirely. And the cost difference? It’s huge.
What’s the real price gap?
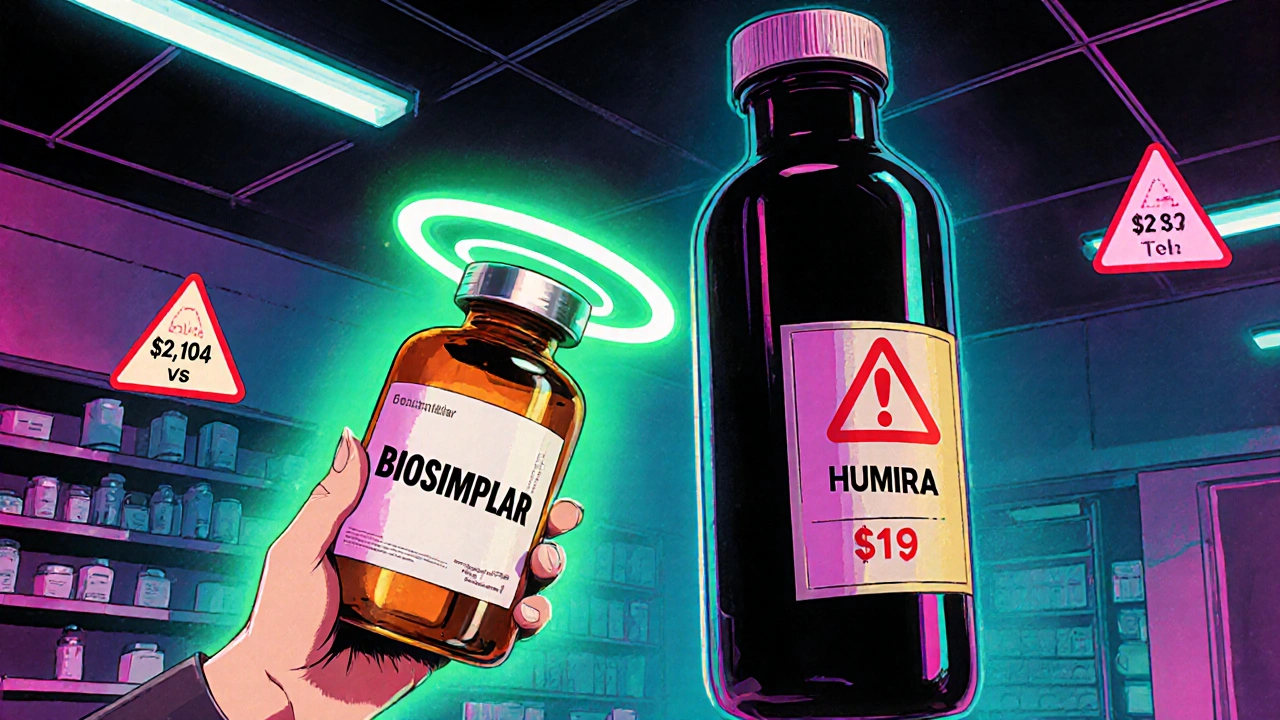
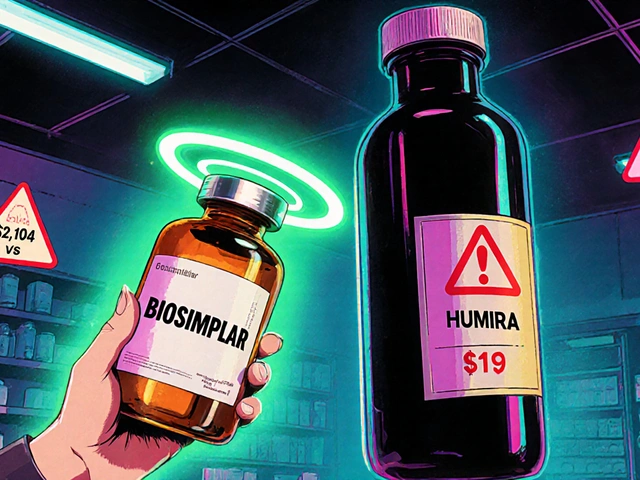
In 2025, the average 30-day prescription for a brand biologic cost $2,104. The biosimilar version? $919. That’s more than half off. For patients on monthly treatments-like those with rheumatoid arthritis, Crohn’s disease, or psoriasis-that’s a savings of over $1,400 every month. Over a year, that’s more than $17,000. And that’s just one drug. Take Humira, for example. Before biosimilars hit the market, it cost about $80,000 per patient per year in the U.S. After biosimilars launched in 2023, the price dropped by 80%. Today, many patients pay less than $16,000 a year for the same treatment. Sandoz’s Hyrimoz alone now holds 14% of the market. And that’s just one biosimilar among 76 approved by the FDA as of October 2025. The savings don’t stop there. When biosimilars enter the market, even the original brand drug often lowers its price. On average, brand biologics drop 25-33% after a biosimilar launches. That’s not just a win for patients-it’s a win for insurers, Medicare, and Medicaid. In 2024 alone, biosimilars saved the U.S. healthcare system $20 billion. Since 2015, total savings have hit $56 billion, according to the Department of Health and Human Services.Why aren’t biosimilars everywhere yet?
You’d think with savings like this, everyone would switch. But they don’t. And the reason isn’t about safety or effectiveness. The FDA says biosimilars are as safe and effective as the originals. The problem is the system. Brand drug companies have built walls around their products. They file dozens of patents-not to protect innovation, but to block competition. These are called “patent thickets.” A single biologic might have over 100 patents covering minor changes in delivery, packaging, or dosing. Each one can delay a biosimilar by years. Then there are Pharmacy Benefit Managers (PBMs). These middlemen negotiate rebates with drugmakers. But here’s the catch: the bigger the rebate, the more they get paid. So if a brand biologic gives a PBM a 30% rebate, and a biosimilar only offers 15%, the PBM has a financial incentive to keep you on the more expensive drug-even if it costs you more out of pocket. That’s why out-of-pocket costs for biosimilars are only 23% lower than brand biologics, even though the wholesale price is over 50% lower. Your insurance plan might cover the biosimilar, but if the rebate structure favors the brand, your pharmacy might not even offer it.
Who benefits from the cost difference?
The biggest winners? Patients. Especially those on long-term treatment. A person with multiple sclerosis on a $15,000-a-month biologic can save $7,000 a month with a biosimilar. That’s life-changing money. Insurers and government programs benefit too. Medicare Part B spends over $30 billion a year on biologics. If just half of those prescriptions switched to biosimilars, Medicare could save $10-15 billion annually. That’s enough to cover free screenings, mental health services, or insulin for millions of diabetics. But the biggest losers? The brand manufacturers. Humira made $21.2 billion globally in 2022. That’s not going to happen again. Biosimilars are eating into their profits. And that’s why they fight so hard to keep them out.What’s changing-and what’s not
The FDA is trying to fix this. In September 2025, they released new draft guidelines to simplify the approval process. They want to cut down on unnecessary clinical trials. Right now, a biosimilar can cost $100-250 million to develop. That’s more than most small drug companies can afford. If the FDA makes it cheaper and faster, more companies will enter the market. The Biden administration’s Biosimilars Action Plan aims to remove rebate walls and push insurers to prioritize lower-cost options. Some states are already requiring pharmacists to substitute biosimilars unless the doctor says no. But progress is slow. Only about 10% of biologics set to lose patent protection in the next 10 years even have a biosimilar in development. Compare that to small-molecule generics-where 90% of prescriptions are generic, and prices drop 79% after competition hits.




Comments
Matthew Mahar
November 22, 2025Okay but like… why are we still letting PBMs call the shots? I had to fight my insurance for THREE MONTHS to get my biosimilar covered. My rheumatoid arthritis didn’t care about their rebate deals. I just wanted to not cry every time I checked my bank account. 😭
John Mackaill
November 23, 2025It’s not just about cost-it’s about access. In the UK, we’ve got biosimilars rolling out faster because the NHS doesn’t play games with rebates. Here in the States, it feels like the system is designed to keep people sick and paying. The science works. The ethics don’t.
Adrian Rios
November 25, 2025Let’s be real-this isn’t just a pharmaceutical issue, it’s a systemic failure of capitalism disguised as healthcare. Brand drug companies aren’t innovating-they’re litigating. They spend more on lawyers than R&D. Patent thickets? That’s not protection, that’s extortion. And PBMs? They’re not intermediaries-they’re parasites feeding off suffering. The FDA’s new guidelines are a start, but unless we break the rebate model entirely, we’re just rearranging deck chairs on the Titanic. And don’t get me started on how pharmacies are forced to stock the expensive stuff because the PBM’s contract locks them in. This isn’t free market-it’s rigged.
Casper van Hoof
November 26, 2025One must consider the epistemological framework within which biosimilar adoption occurs. The ontological distinction between a generic small molecule and a biosimilar lies not merely in chemical composition, but in the phenomenological perception of efficacy by both clinicians and patients. The market dynamics, while economically rational, are culturally irrational insofar as they prioritize profit over patient autonomy. The structural inertia of institutional actors-PBMs, insurers, and even prescribers-reflects a deeper epistemic closure that resists paradigmatic shift.
Richard Wöhrl
November 28, 2025Important note: biosimilars aren't just cheaper-they're just as safe. The FDA requires them to meet the same rigorous standards as the originator drug. And yes, the 80% price drop on Humira? Real. And yes, the $20B saved in 2024? Documented. But here's the kicker: many doctors still don't know the difference between 'generic' and 'biosimilar.' So they default to the brand. And pharmacists? Often can't substitute unless the prescriber allows it. So even if your plan covers it, you might not get it. Ask for it. Demand it. And if your doctor says 'it's not the same,' ask them to show you the data. The data says: it is.
Pramod Kumar
November 29, 2025Bro, imagine paying $15k/month for a drug when you could pay $8k and get the same effect. That’s not a savings-that’s a miracle. In India, we know what it’s like to choose between medicine and rice. Here, people are fighting over rebates while others are skipping doses. This isn’t healthcare-it’s a horror show with a corporate logo.
Brandy Walley
November 30, 2025Ugh so what now we’re supposed to feel bad for pharma companies? They made billions off people’s suffering. Now they’re mad because someone finally figured out how to make it cheaper? Get over it. I’m not paying $2000 a month for a drug that’s now $900. I’m switching. And if my insurance won’t cover it? I’m going cash. No more guilt trips.
shreyas yashas
December 1, 2025My uncle’s on a biosimilar for psoriasis. Paid $400 out of pocket last month. Before? $2200. He cried when he saw the receipt. Not from sadness-from relief. This isn’t politics. This is life. If we can fix this, we should. No excuses.
Write a comment