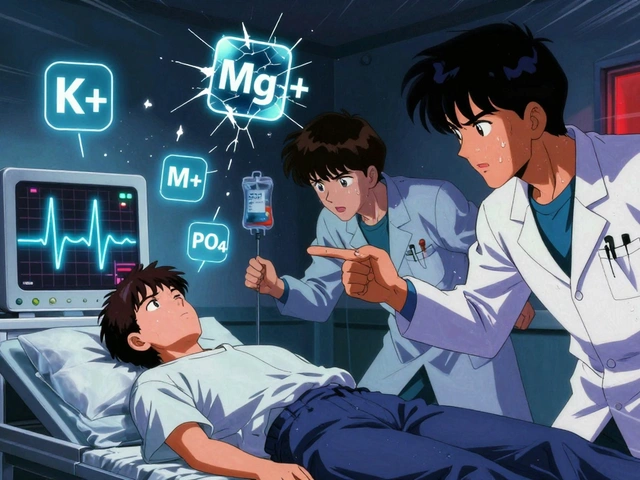
When your body’s electrolytes are out of balance, it doesn’t just mean you feel tired or crampy. Low potassium, low phosphate, or low magnesium can trigger heart rhythms that could stop your heart. High levels can paralyze your breathing. These aren’t minor lab quirks-they’re life-or-death situations, especially in people with kidney disease. And yet, too many patients slip through the cracks because the connections between these three electrolytes aren’t taught well-or worse, ignored.
Why These Three Matter More Than You Think
Potassium, phosphate, and magnesium don’t work alone. They’re locked in a delicate dance. If one is off, the others follow-often in ways that make treatment harder. Take potassium. It keeps your heart beating regularly. But if magnesium is low, giving potassium won’t fix the problem. Your kidneys just keep dumping it out. Same with phosphate. When levels drop too low, your muscles, including your diaphragm, can’t contract properly. You stop breathing. And magnesium? It’s the hidden player in over 300 enzyme reactions. Without it, your cells can’t make energy, your nerves misfire, and your heart becomes unpredictable.
Normal ranges are tight:
- Potassium: 3.2-5.0 mEq/L
- Magnesium: 1.7-2.2 mg/dL
- Phosphate: 2.5-4.5 mg/dL
But danger zones are even narrower. Potassium below 3.0 or above 6.5 mEq/L? That’s an emergency. Magnesium under 1.0 or over 2.5 mg/dL? Same. Phosphate below 1.0 mg/dL means your body is starving for energy. These aren’t just numbers-they’re warning signs.
The Hidden Link: Why Magnesium Comes First
Here’s the most overlooked rule in electrolyte management: check magnesium before you replace potassium. If you don’t, you’re wasting time-and risking your patient’s life.
Hypomagnesemia causes the kidneys to lose potassium, no matter how much you give. It also makes the heart more sensitive to arrhythmias. Studies show that when low potassium and low magnesium happen together, the risk of dangerous heart rhythms jumps dramatically. In fact, treating low potassium without fixing magnesium first often fails. The potassium level might bounce up briefly, then crash again. That’s why top hospitals like Vanderbilt University Medical Center now require magnesium to be repleted before any potassium infusion.
How much magnesium? A single 4-gram dose, given as a 100 mL IV piggyback infused at 1 gram per minute, is standard. Faster than that, and you risk low blood pressure. Slower, and you delay recovery. After giving it, wait 30 minutes and recheck magnesium. If it’s still low, give another 2 grams. Don’t rush. Don’t guess. Just follow the protocol.
When Potassium Goes Too High: The Emergency Protocol
High potassium-hyperkalemia-is the silent killer. It doesn’t always cause symptoms until the heart starts to fail. ECG changes like peaked T waves, widened QRS, or sine wave patterns mean you have minutes, not hours, to act.
The American Heart Association’s 2023 guidelines lay out a clear, step-by-step approach:
- Stabilize the heart with 10-20 mL of 10% calcium gluconate IV. This doesn’t lower potassium-it protects the heart from its effects. Lasts 30-60 minutes.
- Shift potassium into cells with 10 units of regular insulin and 50 grams of dextrose. Works in 15-30 minutes. Watch blood sugar-hypoglycemia is common.
- Remove potassium with potassium-binding resins like patiromer or sodium zirconium cyclosilicate. These are newer, safer alternatives to old-school kayexalate. They bind potassium in the gut and flush it out in stool. Approved by NICE in early 2023.
- Use dialysis if the patient has kidney failure, or if potassium stays above 7 mEq/L despite other treatments.
Monitoring is non-negotiable. After treatment, check potassium at 1 hour, 2 hours, 4 hours, 6 hours, and 24 hours. A drop from 6.8 to 5.5 might look good-but if it jumps back to 6.2 by hour 8, you missed the root cause. That’s why many ERs now use point-of-care testing. It cuts time-to-treatment by 37 minutes on average.

Phosphate: The Forgotten Energy Source
Low phosphate doesn’t always show up on a basic panel. But in critically ill patients-those on ventilators, in ICU, or recovering from surgery-it’s a silent crisis. When phosphate drops below 1.0 mg/dL, muscles weaken. The diaphragm can’t push air in. Patients start suffocating-even if their lungs are fine.
Common causes? Refeeding syndrome after starvation, long-term use of phosphate-binding meds (like those for kidney disease), vitamin D deficiency, and alcoholism. But there’s a newer, surprising cause: iron infusions. In 2020, the FDA warned that high-dose ferric carboxymaltose can cause severe, prolonged hypophosphatemia. It’s not rare-it’s expected in up to 20% of patients after multiple doses.
How to fix it? For mild cases (phosphate 1.5-2.0 mg/dL), oral phosphate works: 8 mmol per dose, three times a day. For severe cases (below 1.0 mg/dL), you need IV. Typical dose: 7.5 mmol in 250 mL of fluid over 4-6 hours. Never rush it. Too fast, and you trigger calcium to drop, leading to tetany or seizures. Monitor calcium every 4-6 hours during replacement.
And watch for rebound. After you fix phosphate, your body may overcorrect. Check levels daily for 2-3 days. Many ICUs now have protocols that trigger phosphate checks every 12 hours in high-risk patients.
Hypermagnesemia: Rare, But Deadly
Too much magnesium? That’s rare outside of kidney failure or overdose. But when it happens, it’s dangerous. Symptoms start with nausea and flushing. Then muscle weakness. Then loss of reflexes. Then breathing stops. Heart rate slows. Blood pressure crashes.
First step: stop all magnesium. That includes antacids, laxatives, and IV infusions. Then give 10-20 mL of 10% calcium gluconate IV. Calcium reverses magnesium’s effect on nerves and muscles. It’s not a cure-but it buys time.
If kidneys are working, give furosemide to flush out excess. If not, dialysis is the only option. Don’t wait. If someone’s not breathing, don’t delay. Get dialysis ready now.

Who’s at Risk-and How to Catch It Early
You don’t need to wait for someone to crash. Screening saves lives.
- All hospitalized patients with kidney disease should get a full electrolyte panel on admission.
- Anyone on diuretics, ACE inhibitors, or ARBs? Check potassium and magnesium weekly.
- Patients on iron infusions? Check phosphate before, 24 hours after, and again at 7 days.
- Those with eating disorders, alcoholism, or recent surgery? Monitor phosphate daily for 72 hours.
Hospitals that use standardized order sets and clinical decision tools have cut electrolyte-related errors by over 22%. That’s not luck. That’s systems.
What’s Changing in 2025
The field is moving fast. New potassium binders like sodium zirconium cyclosilicate are now first-line. Point-of-care testing is in most ERs. And the biggest shift? Personalized medicine.
Genetic factors influence how your kidneys handle potassium and magnesium. Phase 3 trials are wrapping up on genotype-guided replacement protocols. In the next year, doctors may be able to say: “Your gene variant means you lose potassium faster than average. We’ll start you on a maintenance dose before you even get sick.”
For now, stick to the basics: check magnesium before potassium. Know the emergency steps for high potassium. Watch phosphate in the critically ill. And never treat one electrolyte in isolation.
These aren’t just lab values. They’re the rhythm of life. Get them right, and you prevent cardiac arrest, respiratory failure, and death. Get them wrong, and you miss the warning signs-until it’s too late.





Comments
Karl Barrett
December 5, 2025What’s wild is how these electrolytes aren’t just lab values-they’re a triad of physiological interdependence. Magnesium is the unsung conductor here. Without it, potassium is a soloist with no sheet music, phosphate is a battery with no charge circuit. The body doesn’t treat them as separate entities; it treats them as a symphony. When you fix one without the others, you’re tuning the violin while the cello’s string snaps. And yeah, the Vanderbilt protocol isn’t just protocol-it’s clinical wisdom honed by repeated near-fatalities. This isn’t medicine by checklist. It’s medicine by understanding the dance.
Ben Choy
December 6, 2025👏 this is the kind of post that reminds me why I went into critical care. So many of us get bogged down in protocols and forget the *why*. The magnesium-potassium-phosphate triad? It’s like trying to fix a leaky roof without checking the foundation. I’ve seen patients crash because someone just threw KCl at the problem. Took me 3 months of pushing for a lab protocol change on my unit to get magnesium checked before any K+ infusion. Worth it. Every. Single. Time.
val kendra
December 7, 2025just checked my last 3 ICU patients' mg levels before their k+ orders. all were low. saved one from a VTAC this week. you’re right. stop guessing. start checking. 💪
Bill Wolfe
December 8, 2025It’s almost comical how many clinicians still treat electrolytes like they’re isolated variables in a spreadsheet. The fact that we’re even *debating* whether to check magnesium before potassium in 2025 is a reflection of how deeply fragmented medical education has become. I’ve seen residents write ‘K+ 2.8 - give 40 mEq’ without a single thought to Mg or PO4. And then wonder why the patient codes 4 hours later. It’s not negligence-it’s ignorance dressed up as routine. The FDA warning on iron infusions? That’s just the tip of the iceberg. We need mandatory electrolyte competency exams. Not optional. Mandatory.
michael booth
December 9, 2025Thank you for this comprehensive and clinically grounded overview. The emphasis on systems-based interventions-standardized order sets, decision tools, and point-of-care testing-is precisely where modern healthcare must evolve. The 22% reduction in electrolyte-related errors is not merely statistically significant; it is ethically imperative. I have implemented a similar protocol in my institution, and the reduction in ICU admissions for arrhythmias has been remarkable. Let us not underestimate the power of structure in saving lives.
Shofner Lehto
December 11, 2025Hyperkalemia protocol is spot on. Calcium gluconate first-always. I’ve seen teams waste 20 minutes trying to push insulin before stabilizing the heart. Bad idea. And yes, point-of-care testing cuts time. We started using the i-STAT in our ER last year. Time from blood draw to treatment dropped from 52 to 15 minutes. That’s a 70% reduction. Lives saved. Not just numbers.
Jake Deeds
December 12, 2025Oh wow. Someone actually wrote something useful for once. I’ve been screaming about this for years. You know who doesn’t get this? The guy who orders KCl without checking Mg. He’s the same guy who thinks ‘normal range’ means ‘safe.’ Spoiler: it doesn’t. I’ve watched three patients die because someone thought ‘it’s just a lab value.’ I don’t care if you’re a third-year med student or a chief resident. If you don’t check magnesium before potassium, you’re not a doctor-you’re a liability with a stethoscope.
Alex Piddington
December 14, 2025Excellent summary. I particularly appreciate the inclusion of the 2023 AHA guidelines and the mention of newer agents like sodium zirconium cyclosilicate. As a clinical pharmacist, I’ve advocated for these protocols in our formulary since 2022. The shift from kayexalate is long overdue-its side effect profile was unacceptable. Also, the phosphate-iron infusion connection is underappreciated. We now screen all patients receiving ferric carboxymaltose at 24h and 7d. It’s become standard. Thank you for highlighting the systemic change needed-not just individual vigilance.
Emmanuel Peter
December 14, 2025So you’re telling me if I don’t check magnesium before giving potassium, I’m basically a murderer? 😏 I mean, I guess that’s one way to put it. But come on, let’s be real-how many of you actually do this every time? I’ve got 12 patients on my panel and 5 minutes to do rounds. Do you think I’m checking Mg on every single one? Nah. I’m checking the big stuff. And if someone codes? Well… that’s why we have codes, right? 😅
Write a comment