What Is Addison’s Disease?
Addison’s disease is a rare but serious condition where your adrenal glands don’t make enough of two vital hormones: cortisol and aldosterone. These hormones help your body handle stress, control blood pressure, balance salt and water, and regulate metabolism. Without them, even a simple cold can turn life-threatening.
It’s called primary adrenal insufficiency because the problem starts in the adrenal glands themselves - usually because the immune system mistakenly attacks and destroys them. This autoimmune damage doesn’t happen overnight. By the time symptoms show up, about 90% of the adrenal tissue is already gone. That’s why it often goes undiagnosed for years.
First described in 1855 by Dr. Thomas Addison in London, the disease was once mostly caused by tuberculosis. Today, in the U.S. and Europe, over 80% of cases are autoimmune. People with Addison’s often have other autoimmune conditions too - like Hashimoto’s thyroiditis, type 1 diabetes, or vitiligo. About half of all patients develop at least one other autoimmune disorder.
How Do You Know You Have It?
The symptoms of Addison’s disease creep in slowly. Fatigue, muscle weakness, weight loss, and low blood pressure are common. But one sign you won’t miss is darkening skin - especially in folds, scars, gums, and knuckles. That’s because high levels of ACTH (the hormone that tells your adrenals to work) also stimulate pigment cells. It’s not a tan. It’s a sign your body is screaming for help.
Other red flags include salt cravings, nausea, dizziness when standing up, and low blood sugar. Many people are misdiagnosed for years. A 2023 study found that 63% of patients saw at least three doctors before getting the right diagnosis. Gastroenterologists and primary care providers are often the first to see these patients because symptoms mimic stomach bugs or chronic fatigue.
The gold standard test is the ACTH stimulation test. You get a shot of synthetic ACTH, and your cortisol levels are checked before and 30-60 minutes later. If your cortisol doesn’t rise above 18 mcg/dL, your adrenals aren’t responding - confirming adrenal insufficiency. Blood tests also show low sodium, high potassium, and high ACTH levels. A positive test for 21-hydroxylase antibodies confirms the autoimmune cause in most cases.
Why Steroid Replacement Isn’t Optional
There’s no cure for Addison’s disease. But with the right treatment, you can live a full life. The goal is simple: replace what your body can’t make.
You need two types of steroid replacements:
- Glucocorticoids - usually hydrocortisone (Cortef) - to replace cortisol. Typical daily dose is 15-25 mg, split into two or three doses. The biggest dose is taken in the morning to mimic your body’s natural rhythm.
- Mineralocorticoids - usually fludrocortisone - to replace aldosterone. Most people take 50-300 mcg daily. This helps keep sodium up, potassium down, and blood pressure stable.
Unlike secondary adrenal insufficiency (which comes from pituitary problems), Addison’s patients must take both. Skip fludrocortisone, and you risk dangerous electrolyte imbalances.
Cost is a real barrier. Without insurance, hydrocortisone can run $350-$500 a month. A 2022 survey found 40% of patients skip doses or ration pills because of cost. That’s deadly. Under-replacement increases your risk of adrenal crisis by 200%.

Adrenal Crisis: The Emergency You Must Prepare For
An adrenal crisis is a medical emergency. It can kill you within hours if untreated. Symptoms include severe vomiting, abdominal pain, confusion, low blood pressure, and loss of consciousness. Infection, illness, surgery, or even emotional stress can trigger it.
Studies show people with Addison’s have 8-10 adrenal crises per 100 patient-years. That’s far higher than those with secondary insufficiency. And 18% of crises happen because someone missed their meds.
The key to survival is preparation:
- Carry an emergency injection kit with 100 mg of hydrocortisone. Know how to give it - intramuscularly, into your thigh.
- Wear a medical alert bracelet or necklace. Paramedics need to know immediately.
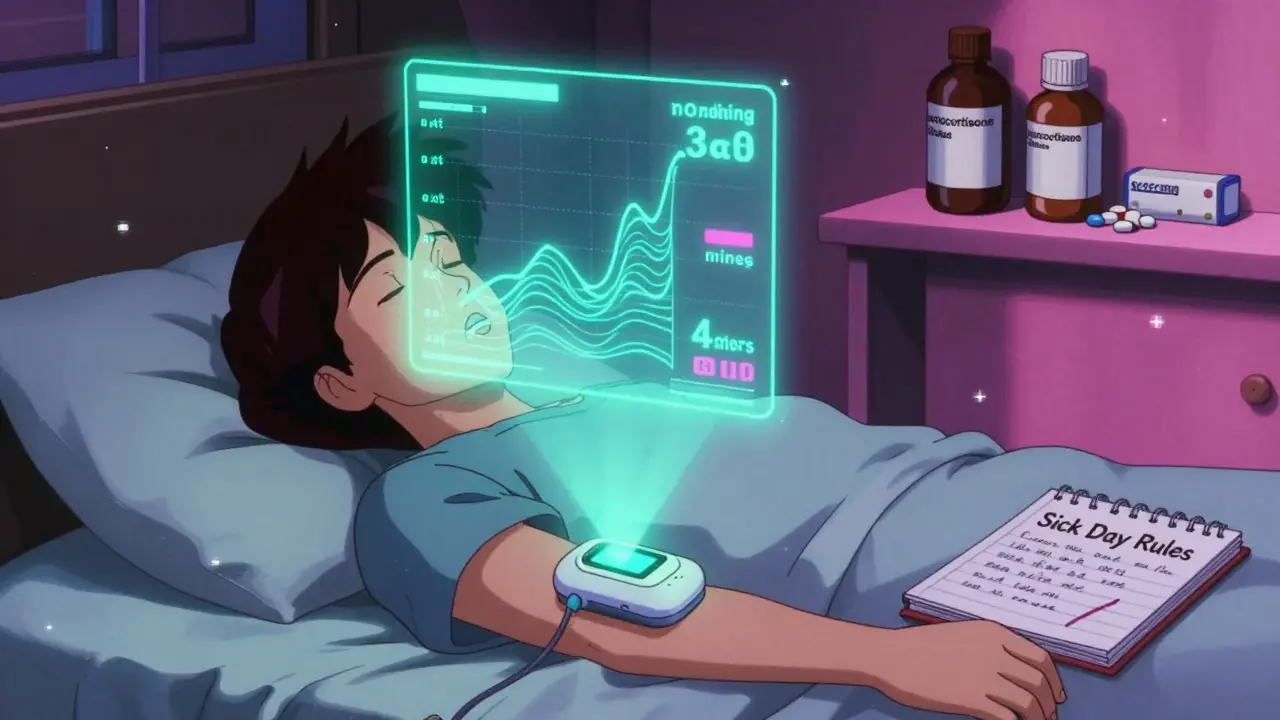
- Follow “sick day rules.” If you’re sick, feverish, vomiting, or injured, double or triple your hydrocortisone dose. If you can’t keep pills down, use the injection.
Delaying treatment increases death risk by 3-5% per hour. There’s no time to wait for test results. If you suspect a crisis, give the shot and call 911.
Living With Addison’s: Daily Challenges and Real-Life Struggles
Managing Addison’s isn’t just about taking pills. It’s about constant vigilance.
Patients on Reddit and support groups talk about the mental toll. One user wrote: “The fear of crisis during every fever is exhausting.” Another said, “Finding a doctor who gets that I need to take extra hydrocortisone at 3 a.m. during a fever? Nearly impossible.”
Even small things become complicated. A dental cleaning? You might need an extra 25-50 mg of hydrocortisone. A flu shot? Double your dose for 24 hours. A vacation? Pack extra meds, keep them cool, and know where the nearest ER is.
And it’s not just physical. Chronic steroid use can lead to weight gain, mood swings, and bone thinning. Over-replacement raises heart disease risk by 44%. Under-replacement makes you vulnerable to sudden death. The balance is razor-thin.
Patients who complete the Addison’s Disease Self Help Group’s “Sick Day Rules” training cut their crisis rates by 85%. Education saves lives.
New Treatments on the Horizon
For decades, hydrocortisone tablets were the only option. But they don’t mimic your body’s natural cortisol rhythm - which peaks in the morning and drops at night. That’s why many patients still feel tired or crash in the afternoon.
In 2023, the FDA approved Chronocort, a modified-release hydrocortisone taken once daily. It releases cortisol slowly, matching your body’s pattern better. In trials, it reduced cortisol swings by 37% and improved energy levels.
Even more promising? Continuous cortisol monitors. Devices now in phase 2 trials can track your cortisol levels in real time, like a glucose meter for adrenal patients. Experts predict these could cut crisis rates by 60% within five years.
And testing is getting smarter. Now, all newly diagnosed patients are routinely tested for 21-hydroxylase antibodies. With 98% accuracy, it confirms autoimmune Addison’s early - helping guide long-term care and screen for other autoimmune conditions.
What You Need to Do Right Now
If you’ve been diagnosed with Addison’s disease:
- Get your emergency injection kit and medical alert ID - today.
- Learn your sick day rules. Double your dose at the first sign of illness. Triple it if you’re vomiting.
- Find an endocrinologist who specializes in adrenal disorders. General practitioners often don’t know the nuances.
- Join a support group. The Addison’s Disease Self Help Group offers free training and resources.
- Get screened for other autoimmune conditions - thyroid, diabetes, B12 deficiency.
If you think you might have Addison’s - fatigue, dark skin, low blood pressure, salt cravings - ask your doctor for an ACTH stimulation test. Don’t wait. Misdiagnosis is common. But early diagnosis saves lives.
Global Patterns and Access Issues
Addison’s disease affects about 10-14 people per 100,000 worldwide. But causes vary by region. In North America and Europe, autoimmune destruction is the main cause. In parts of Africa and Asia, tuberculosis still accounts for more than half of cases.
Access to treatment isn’t equal. In the U.S., 25% of patients ration their meds due to cost. In low-income countries, hydrocortisone is often unavailable. The global adrenal insufficiency market is growing - but not fast enough for those who need it most.
Life expectancy for people with Addison’s is still 3-11 years shorter than average - mostly due to adrenal crises or heart problems from long-term steroid use. But with better drugs, better monitoring, and better education, that gap is starting to close.








Comments
Donna Macaranas
February 2, 2026I’ve been living with Addison’s for 12 years and still get teary-eyed reading posts like this. It’s rare to see the everyday struggles laid out so clearly - the 3 a.m. dose panic, the salt cravings that feel like a betrayal of your willpower, the way your body screams for balance when the world moves too fast. You’re not alone.
Rachel Liew
February 3, 2026Thank you for writing this. I’m a nurse and I’ve had patients with Addison’s who didn’t know how to use their emergency shot. I wish every provider had a copy of this to hand out. The sick day rules? Non-negotiable. And yes, the cost is brutal - I’ve seen people choose between insulin and hydrocortisone. This isn’t just medical. It’s survival.
June Richards
February 4, 2026Why are we still using 1950s-era steroid replacement? Hydrocortisone is a blunt instrument. We’re basically giving people a sledgehammer to fix a watch. Chronocort is a step, but it’s still just a bandaid. What about stem cell therapies? Why isn’t the NIH funding real cures instead of better dosing schedules?
Lisa Rodriguez
February 5, 2026My sister was misdiagnosed for 5 years as having chronic fatigue and IBS. When she finally got tested, her sodium was 128. She was in the ER for three days. I wish I’d known about the dark skin thing - her knuckles looked like she’d been tanning in a booth. She’s doing great now, but it took a miracle to get someone to listen. Please, if you’re tired and craving salt, push for the ACTH test. Don’t let them tell you it’s anxiety.
Lilliana Lowe
February 6, 2026It’s mildly amusing how this post treats Addison’s as if it’s some tragic rarity. It’s not. It’s a manageable endocrine disorder - albeit one with a steep learning curve. The real tragedy is the proliferation of fear-mongering language like 'screaming for help' and 'life-threatening cold.' Cortisol replacement is effective, predictable, and well-studied. The emotional dramatization does more harm than good to patient autonomy.
Chris & Kara Cutler
February 7, 2026GET YOUR EMERGENCY KIT TODAY. 💪💉
Angel Fitzpatrick
February 9, 2026Did you know the adrenal glands are controlled by the pineal gland, which is affected by 5G radiation? Big Pharma doesn’t want you to know that cortisol production can be restored with magnesium and grounding - but they profit off your dependency on synthetic steroids. The WHO quietly removed adrenal crisis from their list of reportable diseases in 2019. Coincidence? I think not.
Nidhi Rajpara
February 10, 2026This is a meticulously researched article with precise clinical terminology and logical structure. The distinction between primary and secondary adrenal insufficiency is correctly delineated, and the reference to 21-hydroxylase antibodies as a diagnostic marker is both accurate and appropriately contextualized. However, the inclusion of anecdotal Reddit quotes introduces an element of subjectivity that, while emotionally resonant, may compromise the article’s scholarly integrity. The cost disparity section, while compelling, lacks citation of peer-reviewed economic analyses. Nonetheless, the overall contribution to patient education is commendable.
vivian papadatu
February 11, 2026I’m from India and we don’t have access to Chronocort or even reliable hydrocortisone in rural areas. My cousin died because the pharmacy ran out of fludrocortisone for three weeks. No one told her to double her dose when she got sick. I’m so glad this exists, but it feels like a luxury for people in the US. We need global access, not just better meds. 🌍
Lu Gao
February 11, 2026Actually, Addison’s isn’t autoimmune in most cases outside the West - it’s TB. So this whole post is basically a Western-centric narrative. And calling it 'rare' is misleading when in parts of Africa it’s one of the top causes of death in young adults. Also, why are we still calling it 'Addison’s disease'? It’s adrenal insufficiency. The name is outdated and colonial. Just saying.
Bryan Coleman
February 12, 2026Just wanted to add - if you’re on hydrocortisone and feel like you’re always tired even on dose, talk to your endo about cortisol rhythm. Mine was off too - we switched to three doses a day and it changed everything. Also, wear the bracelet. I forgot mine once during a hike and my partner had to explain it to the EMTs. They didn’t believe me until I showed them the prescription bottle. Don’t make them guess.
Write a comment