Every year, around 125,000 people in the U.S. die because they don’t take their mental health medications as prescribed. That’s more than traffic accidents or gun violence. Yet this problem stays quiet. No headlines. No viral posts. Just people stopping their pills, feeling worse, and ending up in emergency rooms - again and again.
Why People Stop Taking Their Medications
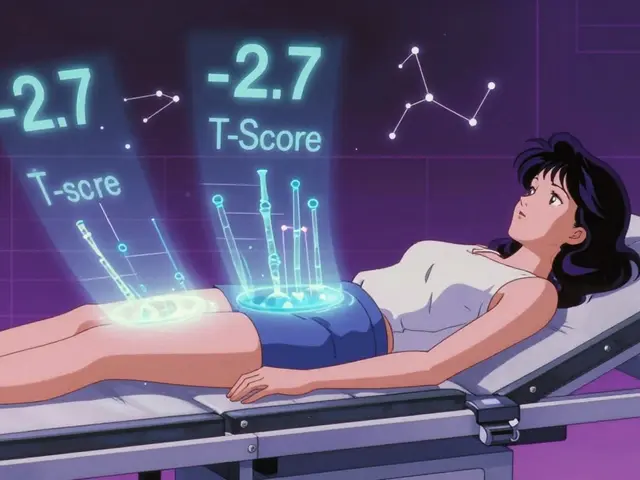
It’s not about being lazy or irresponsible. People stop taking psychiatric meds for real, complicated reasons. One big factor is side effects. Weight gain, drowsiness, shaking, or feeling emotionally numb - these aren’t minor inconveniences. They change how you see yourself. A woman on antipsychotics told her doctor she felt like a "zombie," so she stopped. Two weeks later, she was hospitalized for psychosis. Another reason is lack of insight. If you don’t believe you’re sick, why take a pill? This is common in schizophrenia and bipolar disorder. You might feel fine - until you’re not. Then there’s cost. A monthly supply of antipsychotics can run $300-$800 without insurance. Even with coverage, copays add up. One patient in San Francisco skipped doses to stretch her pills, saying, "I’d rather be sick than broke." Dosing complexity matters too. Taking four pills a day? That’s hard to remember. A 2024 study found patients on once-daily regimens were 67% more likely to stick with treatment than those on multiple daily doses. And let’s not forget stigma. People hide their meds. They flush them. They lie to their families. "I don’t need those," they say. But what they really mean is, "I’m ashamed."What Works: The Proven Solutions
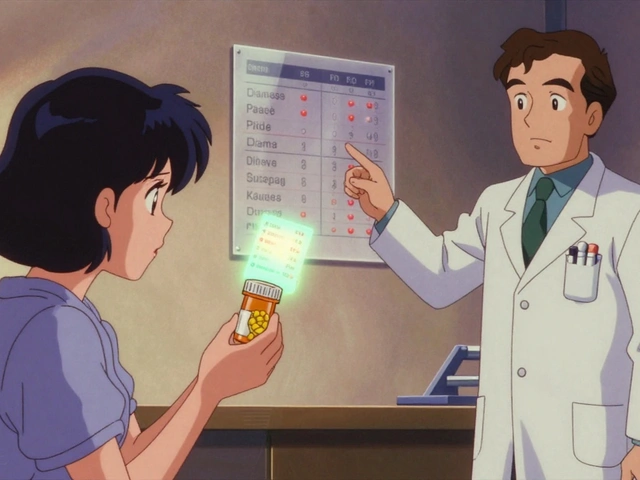
The good news? We know what helps. Not guesswork. Not apps that ping you to take your pill. Real, tested strategies backed by data. Pharmacist-led care is the most effective approach. Not just handing out bottles - active collaboration with psychiatrists. In a 2025 study published in Frontiers in Psychiatry, patients working with a pharmacist-psychiatrist team saw a 142% greater improvement in adherence than those getting standard care. How? Pharmacists check in weekly. They adjust doses. They talk about side effects without judgment. They find cheaper alternatives. One patient in Ohio had his medication switched from a $700/month brand to a $40 generic - and stayed on it. Simplifying the regimen is powerful. If you can take one pill instead of three, you’re far more likely to do it. A NAMI survey showed 87% of patients stayed adherent with once-daily dosing, compared to just 52% with multiple daily doses. Yet 73% of patients said their doctor never even asked if they could simplify things. Addressing symptoms that block adherence works better than generic reminders. If someone feels worthless, they think, "Why bother?" If they’re suicidal, they might stop meds to "end it faster." Treating those feelings - not just the psychosis or depression - makes adherence stick. A 2023 study found that patients who received targeted counseling for hopelessness improved adherence by 41%, even without changing their meds. Long-acting injectables are changing the game. For schizophrenia, monthly or bi-monthly shots have an 87% adherence rate - compared to 56% for daily pills. They’re not perfect. Some patients hate needles. But for those who can’t manage pills, it’s life-changing. The FDA now highlights these as key tools for improving outcomes.What Doesn’t Work (And Why)
Most digital apps? They’re not enough. A 2024 review found medication reminder apps improved adherence by just 1.8% for psychiatric meds - statistically insignificant. Why? Because they don’t fix the root causes. You can’t text your way out of stigma, cost, or lack of insight. Punitive measures? No. Threatening to cut off care if you miss doses? That drives people away. Same with shaming. "You’re not trying hard enough" is the last thing someone struggling with mental illness needs to hear. Generic education pamphlets? Useless. Telling someone "meds help you feel better" doesn’t work if they feel worse on them. You need personalized, ongoing conversations - not brochures.
Real Systems That Are Making a Difference
Kaiser Permanente in Northern California rolled out a pharmacist-led Medication Regimen Management program. Within 90 days, adherence to antipsychotics jumped 32.7%. Hospitalizations dropped by 18.3%. Their CMS Star Rating went from 3.8 to 4.3. But here’s the catch: 63% of community clinics that tried to copy this failed within a year. Why? They didn’t change workflows. They didn’t train staff. They didn’t pay pharmacists for this work. Successful programs do four things:- Use data to find high-risk patients - like those who miss appointments or have recent ER visits.
- Offer cost transparency - show patients exactly what their meds cost and what alternatives exist.
- Simplify dosing - reduce pills, switch to long-acting shots when possible.
- Train providers to talk about adherence as a shared problem - not a patient failure.
The Hidden Cost of Doing Nothing
Non-adherence doesn’t just hurt individuals. It drains the system. Each year, poor medication adherence adds up to $100-$300 billion in avoidable U.S. healthcare costs. That’s billions in ER visits, hospital stays, and lost productivity. Medicare and Medicaid now tie payments to adherence. CMS’s 2025 MIPS Measure #383 requires tracking Proportion of Days Covered (PDC) for schizophrenia patients. If your clinic’s PDC is below 80%, you lose money. Insurers like UnitedHealthcare now tie 12% of mental health provider pay to adherence targets. Yet the national average for antipsychotic adherence? Just 58.7%. For diabetes? 72.3%. We treat physical chronic illnesses better than mental ones. That’s not just unfair - it’s dangerous.What You Can Do - If You’re a Patient
If you’re struggling to take your meds:- Ask your doctor: "Can we switch to a once-daily pill or shot?"
- Ask your pharmacist: "Is there a cheaper version? Can you help me find assistance programs?"
- Bring up side effects - even if you’re embarrassed. There’s always a workaround.
- Find a support group. Reddit’s r/mentalhealth has 1.2 million members. Many say working with a medication specialist was their turning point.
- Don’t stop cold. Talk to someone first. Tapering safely matters.
What You Can Do - If You’re a Provider or Caregiver
If you work in mental health or care for someone who does:- Stop asking, "Why aren’t you taking your meds?" Start asking, "What’s making it hard?"
- Screen for cost, side effects, and hopelessness - not just symptoms.
- Partner with a pharmacist. Even one hour a week makes a difference.
- Use long-acting injectables when appropriate. Don’t wait for a crisis to suggest them.
- Track adherence like you track blood pressure. Make it part of every visit.






Comments
George Taylor
December 8, 2025So let me get this right: we’ve got a system that’s literally killing people… and the solution is to make pharmacists do more work? Wow. Just wow. You know what else is expensive? Therapy. And counseling. And housing. And food. But nope-let’s just shove more responsibility onto overworked pharmacy staff while the real issue-poverty, trauma, systemic neglect-gets ignored. This isn’t a fix. It’s a Band-Aid on a hemorrhage. And you call this "proven"? I call it performative compassion.
Nikhil Pattni
December 9, 2025I am from India and here we have a different problem: most people don't even know they have mental illness, let alone take medicine for it. In rural areas, people go to astrologers or priests first, not doctors. Even when they do go to doctors, they buy medicines from local chemists without prescription and stop when they feel "better"-which is usually after 2-3 days. The idea of once-daily dosing or long-acting injections? That's a luxury. We need community health workers, not pharmacists with PhDs. Also, why is no one talking about how stigma is worse here? A man was beaten by his own brother for taking antidepressants. So yes, cost and complexity matter-but first, we need to teach people that mental illness is not a curse or a sin.
Arun Kumar Raut
December 10, 2025Hey, I just want to say this: if someone is struggling to take their meds, they’re not lazy. They’re scared. They’re tired. Maybe they feel like a burden. Maybe they’ve been told they’re "crazy" too many times. I’ve been there. What helped me was someone sitting with me-not judging, not pushing, just asking, "What’s one thing that’s making this hard?" That’s it. No apps. No lectures. Just a human being who didn’t look away. And yeah, pharmacists can help. But so can your neighbor. So can your cousin. So can you. We don’t need perfect systems. We just need to stop pretending this is someone else’s problem.
precious amzy
December 10, 2025The entire premise of this article is predicated upon a deeply flawed ontological assumption: that mental illness is a biological entity reducible to pharmacological intervention. One must ask: if psychiatric medications are so efficacious, why is the rate of institutionalization and functional decline unchanged over the past 50 years? The data you cite are statistically significant but epistemologically vacuous. Adherence metrics are not outcomes-they are proxies for control. And control, my dear author, is not care.
Carina M
December 11, 2025I find it profoundly disturbing that this article frames non-adherence as a systemic failure while offering no moral condemnation of the individual who chooses to abandon treatment. There is responsibility here. There is agency. To excuse non-adherence as a product of stigma, cost, or side effects is to infantilize the mentally ill. If one cannot muster the discipline to take a pill, perhaps they are not ready for autonomy. This isn't about equity. It's about lowering standards to accommodate unwillingness.
William Umstattd
December 11, 2025I’ve been in the ER three times because someone stopped their meds cold turkey-and then screamed at the nurses for not ‘understanding’ why they were hallucinating. Let me tell you something: compassion without boundaries is cruelty. Yes, cost is a problem. Yes, side effects suck. But if you’re going to take a drug that alters your brain chemistry, you have a moral obligation to follow the protocol. The fact that we’ve turned this into a social justice issue instead of a medical one is why people keep dying. We don’t let diabetics skip insulin because they ‘feel fine.’ Why are we letting people do this with antipsychotics? It’s not stigma. It’s negligence. And someone needs to say it.
Angela R. Cartes
December 12, 2025I mean… I get it. But also… why is no one talking about how the FDA approves these drugs based on 6-week trials? 🤔 Like… how do you know if something works long-term if you’ve only tested it for 42 days? And then you’re supposed to take it for life? And the side effects? They’re literally worse than the original symptoms. I’m not saying don’t take meds. I’m saying… maybe we’re asking the wrong questions? 🤷♀️
Andrea Beilstein
December 12, 2025The real tragedy isn't that people stop taking pills it's that we've reduced healing to a dosage schedule. The soul doesn't respond to calendars or pharmacy charts. We treat depression like a broken pipe when it's more like a storm inside a house with no windows. The pharmacist can refill the prescription but who will sit with the silence? Who will hold space for the shame that says you're broken even when you're taking the medicine? The system fixes the body while the spirit starves. And we call that progress
Write a comment