SJS/TEN Medication Risk Checker
This tool helps you identify if you're taking medications associated with Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN) risk. SJS/TEN are severe skin reactions that can be life-threatening.
Select any medications you're currently taking:
Risk Results
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) aren’t just rare skin rashes. They’re medication-related emergencies that can turn deadly in days. You might start with a fever, sore throat, or fatigue-like a bad cold. Then, within 1 to 3 days, your skin begins to burn, blister, and peel. Mucous membranes in your mouth, eyes, and genitals break down. What began as a mild reaction can become a full-body crisis. And it all happens fast. If you’re taking certain medications, you need to know the warning signs-because waiting even one day can change your outcome.
What Exactly Is SJS and TEN?
SJS and TEN are two ends of the same dangerous spectrum. They’re both caused by severe immune reactions to drugs, leading to the death of large areas of skin. The difference? How much of your skin is affected.
If less than 10% of your body surface area is involved, it’s called Stevens-Johnson Syndrome. If more than 30% peels off, it’s Toxic Epidermal Necrolysis. Between 10% and 30%? That’s overlap syndrome. In the worst TEN cases, up to 100% of the skin can detach-like a severe burn, but without heat. The skin doesn’t just itch or flake. It dies, then sloughs away in sheets. This isn’t a rash you can treat with cream. It’s a medical disaster.
The condition starts with flu-like symptoms: fever, chills, cough, body aches. Then comes the rash-red or purplish patches that spread quickly. Blisters form. The top layer of skin separates from the layers beneath. It’s painful. It’s terrifying. And it’s often mistaken for a common allergic reaction-until it’s too late.
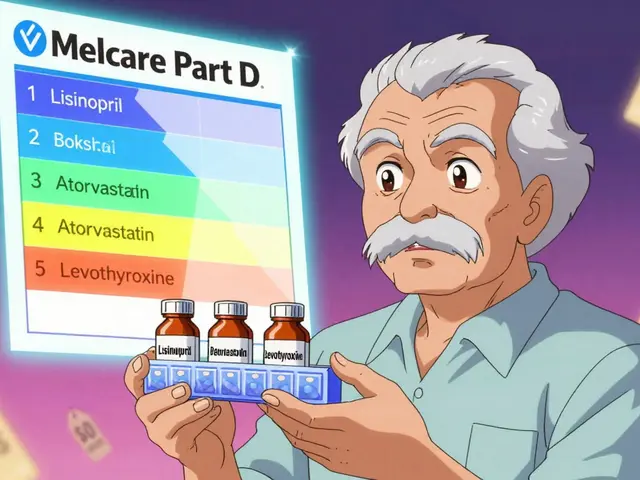
Which Medications Trigger These Reactions?
Not every drug causes SJS or TEN. But some carry a known, documented risk. The most dangerous include:
- Allopurinol (used for gout)
- Lamotrigine (for epilepsy and bipolar disorder)
- Carbamazepine and phenytoin (anti-seizure meds)
- Nevirapine (an HIV drug)
- Penicillin and sulfonamides (like sulfamethoxazole)
- Oxicam NSAIDs (meloxicam, piroxicam)
- Phenobarbital
Here’s the catch: you don’t need to be on the drug for long. Reactions can happen within the first 8 weeks-sometimes even after you’ve stopped taking it. For lamotrigine, the risk spikes if you increase the dose too fast, or if you stop it suddenly and restart without slowly building back up.
And it’s not just the exact drug. If you’ve had a reaction to carbamazepine, you’re at high risk if you later take phenytoin or lamotrigine. These drugs are chemically similar. Your immune system remembers. Survivors must avoid not just the original drug, but entire classes of related medications. This is why doctors ask about past rashes before prescribing.
Who’s at Higher Risk?
SJS and TEN can strike anyone-but some people are more vulnerable:
- People with HIV or weakened immune systems (from chemo or other conditions)
- Those who’ve had a previous skin reaction to anticonvulsants
- People allergic to trimethoprim (a common antibiotic)
- Those taking sodium valproate along with lamotrigine (a dangerous combo)
- People with a family history of SJS/TEN-suggesting genetic links
Genetics play a role. Certain gene variants, like HLA-B*15:02, are strongly tied to carbamazepine-induced SJS in people of Asian descent. Testing for this gene is now standard in some countries before prescribing the drug. If you’re from Southeast Asia and your doctor prescribes carbamazepine, ask if genetic screening is available.
Children are more likely to get SJS than adults-but the condition is still rare overall. Even if you’re on a high-risk drug, your chance of developing SJS/TEN is less than 5 in a million per week. But when it happens, it’s life-altering.
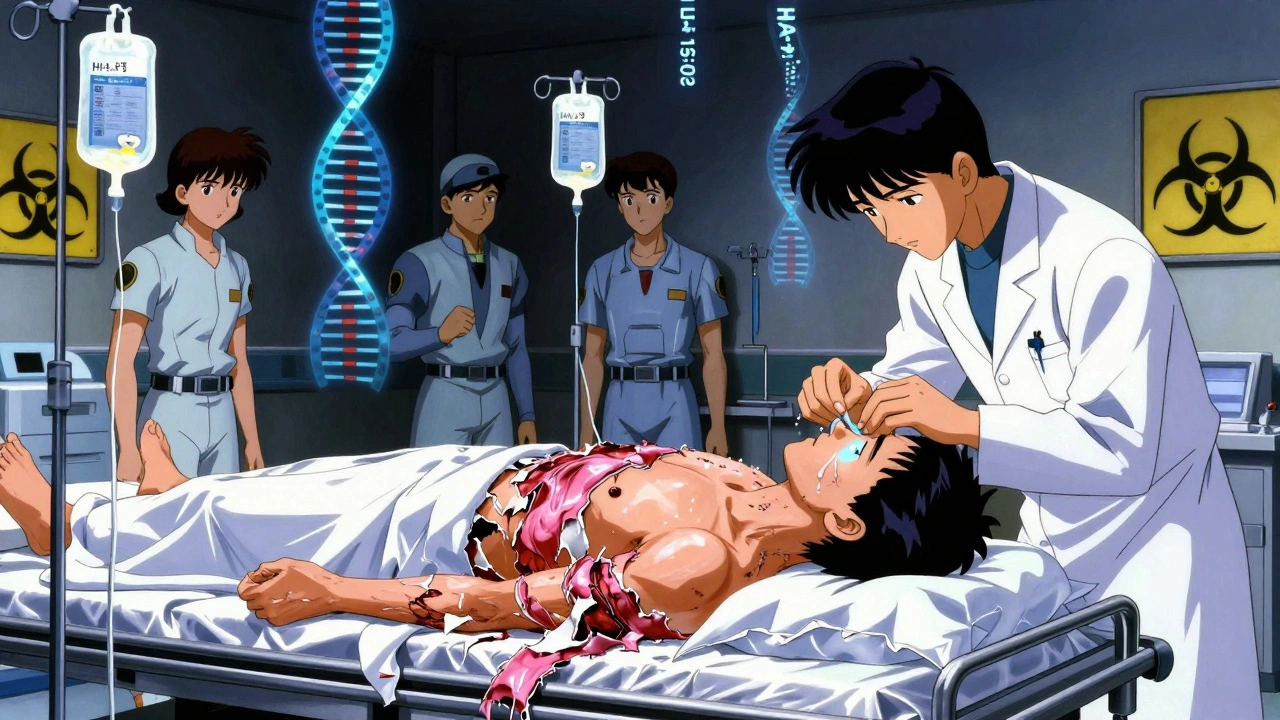
What Happens in the Hospital?
If you suspect SJS or TEN, go to the ER immediately. There’s no home remedy. No over-the-counter fix. Delaying care increases your risk of death.
Once you arrive, the first step is stopping the suspected drug. That’s non-negotiable. Even if you’re not sure which one caused it, doctors will stop all non-essential medications.
You’ll be moved to a burn unit or intensive care unit. Why? Because your skin is gone. Your body is exposed. You lose fluids, heat, and protection from infection. Treatment focuses on:
- Fluid replacement (IV fluids to prevent shock)
- Wound care (special dressings, sterile environments)
- Pain management (often requiring strong opioids)
- Preventing infections (antibiotics if needed, but only if infection is confirmed)
- Eye care (daily saline rinses, ophthalmologist visits)
- Nutritional support (often through feeding tubes, since mouth sores make eating impossible)
There’s no magic drug. Steroids and IVIG (intravenous immune globulin) are sometimes used, but studies show mixed results. The best treatment? Early recognition and expert supportive care.
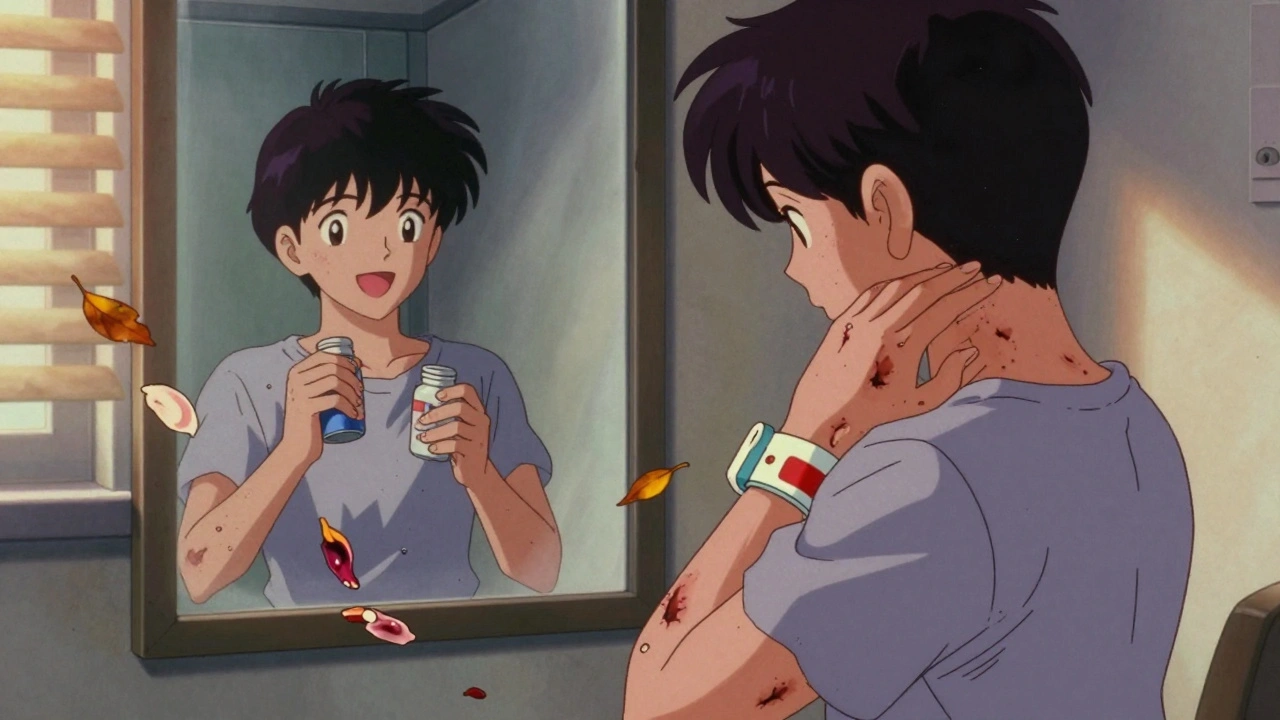
Long-Term Damage Is Common
Surviving SJS or TEN doesn’t mean you’re back to normal. In fact, most survivors face lasting problems.
Up to 50% of people develop serious eye complications: dry eyes, scarring, blurred vision, even blindness. That’s why ophthalmologists see these patients for at least a year after recovery. Some need corneal transplants.
Other long-term issues include:
- Scarring and discoloration of the skin
- Nail loss or deformities (nails often grow back, but slowly)
- Thinning hair or permanent hair loss
- Chronic mouth sores, dry mouth, gum disease
- Esophageal strictures (narrowing that makes swallowing hard)
- For women: vaginal scarring and stenosis (narrowing)
- For men: phimosis (tight foreskin)
Some people develop chronic pain, fatigue, or depression after surviving. The trauma of losing skin, spending weeks in isolation, and facing a long recovery changes you.
And yes-death is possible. Mortality rates: 5% for SJS, up to 30% for TEN. The biggest killers? Sepsis, organ failure, and blood clots.
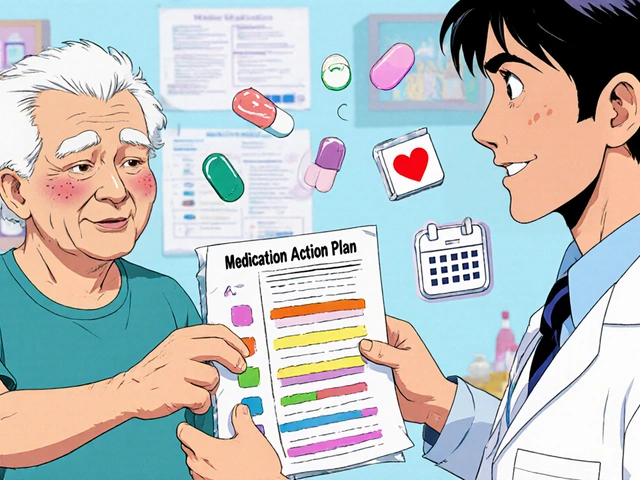
How to Prevent It
You can’t always predict SJS or TEN-but you can reduce your risk.
- If you’re prescribed lamotrigine, carbamazepine, or allopurinol: start low, go slow. Never rush the dose increase.
- Don’t start new medications or supplements during the first 8 weeks of high-risk drugs.
- Know your family history. If a close relative had SJS, tell your doctor.
- Pay attention to your skin. A new rash with blisters or peeling? Go to the ER-not your GP.
- Keep a list of all medications you’ve taken, especially if you’ve had a rash before.
- If you’ve had SJS/TEN before, carry a medical alert card. Never take the same drug-or anything similar-again.
Doctors need to know your history. If you’ve had a rash with one anticonvulsant, don’t assume the next one is safe. Cross-reactivity is real. And if you’re told, "It’s probably just a harmless rash," trust your gut. If it’s spreading, painful, or you’re feeling unwell-get help now.
What to Do If You Think You Have It
Don’t wait. Don’t call your pharmacy. Don’t Google it. If you’re on a high-risk drug and you develop:
- A spreading red or purple rash
- Blisters on skin or inside your mouth
- Peeling skin
- Fever, sore throat, or burning eyes
-go to the emergency room immediately. Say: "I think I might have Stevens-Johnson Syndrome." That phrase gets attention. It triggers the right protocol.
Bring your medication list. If possible, bring the pill bottle. Time matters. The sooner the drug is stopped, the better your chance of survival.
Can SJS or TEN be caused by over-the-counter drugs?
Yes. While most cases are linked to prescription drugs like lamotrigine or allopurinol, over-the-counter NSAIDs like piroxicam and meloxicam have also caused SJS/TEN. Even common pain relievers can trigger a reaction in rare cases, especially if you’ve had a prior skin reaction to them.
How long after taking a drug can SJS/TEN appear?
Most cases start within 1 to 3 weeks of beginning a new drug. But reactions can occur up to 2 weeks after stopping the medication. This is why doctors warn patients to stay alert even after they’ve finished a course of a high-risk drug.
Is SJS/TEN contagious?
No. SJS and TEN are not infections. They’re immune reactions triggered by drugs. You cannot catch it from someone else. But because the skin is damaged and exposed, patients are at high risk of catching infections like sepsis-so they’re kept in sterile environments.
Can you get SJS/TEN from vaccines?
Extremely rare. While some case reports exist, vaccines are not a common cause. The vast majority of SJS/TEN cases are linked to medications, especially anticonvulsants, antibiotics, and gout drugs. Vaccine-related cases are outliers and not considered a significant risk.
What should I do if I’ve had SJS/TEN before?
Never take the same drug again-or any similar one. Keep a medical alert card or bracelet listing the drugs you must avoid. Tell every doctor, dentist, and pharmacist about your history. Cross-reactivity is real, and a second episode is often worse. Survival rates drop sharply with recurrence.
Final Thoughts
SJS and TEN are rare-but when they happen, they’re brutal. The drugs that cause them are often necessary. But they come with hidden risks. If you’re prescribed one of these medications, don’t panic. But do pay attention. Know the signs. Speak up. Your skin is your body’s first line of defense. When it starts to fail, it’s not a nuisance-it’s a cry for help.







Comments
Emily Haworth
December 13, 2025I swear this happened to my cousin after she took ibuprofen for a headache. 😱 They thought it was a rash, then she started peeling like a banana. ER saved her, but she lost her eyelashes and can't cry anymore. 🤕💔
Tyrone Marshall
December 14, 2025This is one of those topics that makes you realize how little we're taught about the hidden dangers of meds. It's not just about side effects-it's about your body turning against you. I've seen patients go from grocery shopping to ICU in 48 hours. The real tragedy? Most doctors don't even know the warning signs until it's too late. We need better public awareness, not just fine print on pill bottles.
Keasha Trawick
December 16, 2025Let me just say-this isn't a rash. This is your epidermis staging a coup. 💥 Imagine your skin becoming a deflated balloon, sloughing off in sheets like wet tissue paper. It's not 'allergic reaction'-it's your immune system going full kamikaze on your entire body. And the worst part? You're told it's 'just a reaction' until you're lying in a burn unit with your corneas exposed. This is medical horror porn-and it's real.
kevin moranga
December 18, 2025I'm so glad someone put this out there. My sister was on lamotrigine and got the rash at week 5-she thought it was heat rash. I made her go to the ER and she’s alive today because of it. Seriously, if you're on any of these meds and feel even a little off, don’t wait. Don’t ‘wait and see.’ Your skin is screaming. Listen. And if you're a doc reading this-please, for the love of God, screen for HLA-B*15:02 if your patient is Asian. It’s not optional. It’s life-saving.
Yatendra S
December 19, 2025The universe whispers warnings... and we ignore them. Allopurinol, lamotrigine... these are not mere chemicals. They are keys to the temple of our immune system. When the temple burns, it is not punishment-it is revelation. We treat medicine like a vending machine. Pop a pill, get relief. But the body remembers. It keeps score. And when it strikes back? It does not knock. It obliterates. We must stop treating biology like a software update.
Webster Bull
December 21, 2025Dude. If you got a rash on one of these meds? ER. Now. No cap. I know someone who waited 3 days. Lost 60% of his skin. Still has scars that look like melted plastic. Don't be that guy.
Tom Zerkoff
December 22, 2025The clinical distinction between SJS and TEN remains critically important for prognostication and resource allocation. While the pathophysiology is conserved across the spectrum, the extent of epidermal detachment directly correlates with mortality risk, fluid loss, and duration of hospitalization. It is therefore imperative that clinicians recognize the early prodrome-fever, mucosal involvement, and rapidly expanding erythematous lesions-as a medical emergency requiring immediate cessation of all non-essential pharmacological agents and transfer to a specialized burn or ICU setting.
Himmat Singh
December 23, 2025This article is alarmist. SJS/TEN is statistically negligible compared to the millions of doses administered daily. The real danger is fearmongering that causes patients to refuse life-saving medications. I’ve seen epileptics stop lamotrigine because of this fear-and then suffer uncontrolled seizures. Risk exists, yes. But it is not an excuse to abandon rational pharmacotherapy. Evidence-based medicine must prevail over emotional narratives.
Jamie Clark
December 24, 2025You people are so naive. This isn't about 'rare side effects.' It's about pharmaceutical companies hiding the truth. They knew allopurinol and lamotrigine caused this for decades. They didn't test properly. They didn't warn enough. And now you're all acting like this is some shocking revelation? Wake up. This is corporate manslaughter dressed up as medical advice. The system is broken. And you're just reading about it like it's a news article. It's a crime scene.
Write a comment